‘Hospital at Home’ Could Be the Future of Health Care. Not Everyone Thinks It’s a Good Idea
‘Hospital at Home’ Could Be the Future of Health Care. Not Everyone Thinks It’s a Good Idea Lindsay Lyon
In July 2022, Rudie Watzig collapsed. The diagnosis was as serious as it was unexpected—cirrhosis of the liver—and it landed him in the intensive care unit for what he considered a period of sheer torture. “I hated it. I hated being in the hospital,” says Watzig, 44, of Portland, Oregon. “Not seeing my kids … not having my wife there … not having my nice Purple mattress to sleep on.”
[time-brightcove not-tgx=”true”]
So imagine his chagrin when he was again rushed to the emergency room a few months later, this time for breathing problems due to fluid buildup around his lungs that needed to be drained with a needle in his back. His heart sank at the thought of another hospitalization stemming from his liver disease—until he was told that once stabilized, he could try something different: hospital at home.
You read that right: inpatient-style care for serious medical issues within the comfort of one’s home. “This isn’t home health light, it is true hospital-level care,” says Colleen Hole, a vice president and chief nurse executive with Atrium Health, a North Carolina-based health system that runs what is thought to be the nation’s largest hospital-at-home program, which Hole oversees. “This model actually delivers care to the patient, like pizza, but way better.”
Hospitals and health systems around the country have been rolling out flavors of “acute hospital care at home” programs as part of a national movement to not only boost the patient experience but to reduce hospital overcrowding and bed shortages, problems that are expected to intensify as more and more baby boomers advance into their senior years.
Exactly how a program works can vary from hospital to hospital and state to state, based on regulatory issues. But generally, a patient lands in the ER or other inpatient unit and is screened to see if they’d be a good fit.
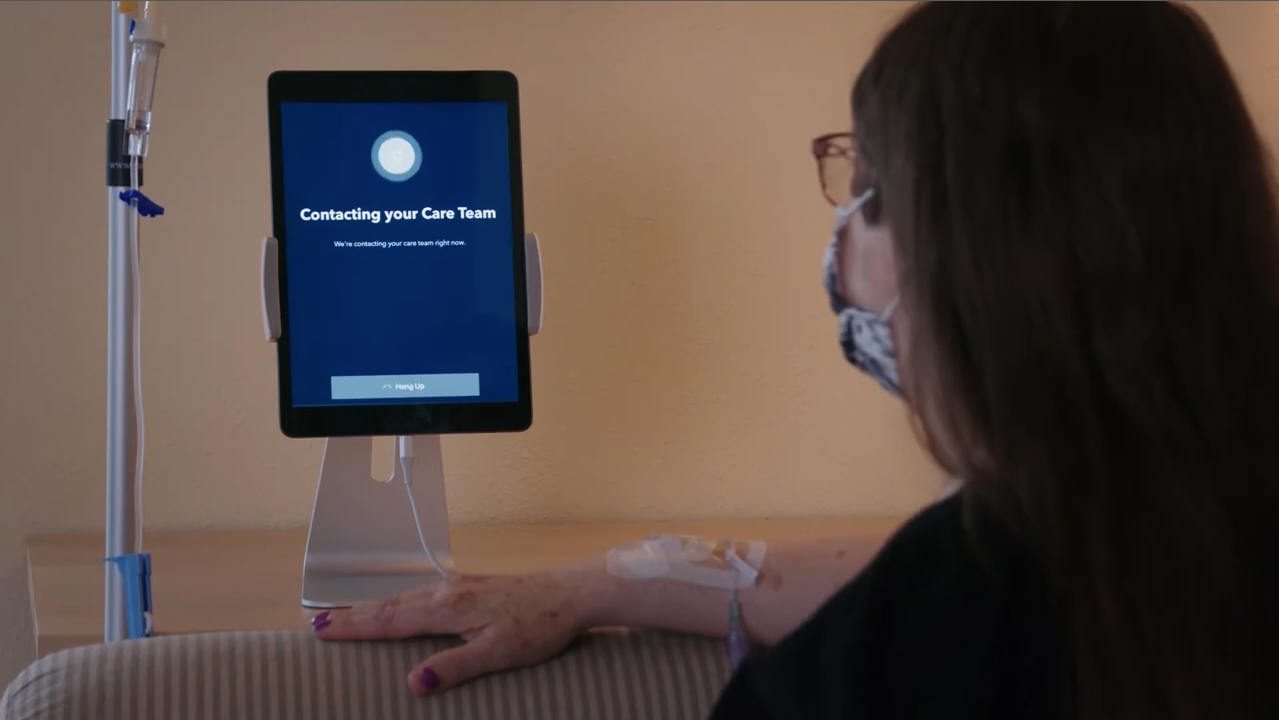
If the answer is yes, and the patient is on board, they are “transferred” home, where they’re met by a professional who sets up everything they need to be monitored on their own turf. This may include a 4G-enabled tablet for video visits with a virtual care team accessible 24/7 at the push of a button; a phone that immediately connects to that team; a wearable device that continually tracks their vital signs; a blood pressure cuff; a pulse oximeter; an emergency alert necklace; and so on.
Patients usually get two in-person exams each day from, for example, a nurse or community paramedic, along with daily video or in-person visits with the doctor leading their care. IV medications can often be administered. Basic lab work can be taken and picked up via courier. Electrocardiograms are possible, as are certain imaging tests like ultrasounds.
“I remember one time, I needed an X-ray of my lungs … so they had this guy—he came over with a frickin’ van, wheeled an X-ray machine into my living room and he put the plate right behind the chair here,” Watzig recalls. “I took an X-ray right where I’m sitting right now … the only thing they couldn’t bring to me was a CT machine.”
At this stage, hospital-at-home programs are being offered to patients who need hospitalization but are stable enough to be cared for safely at home, experts say. Picture everything from heart failure and chronic obstructive pulmonary disease (COPD) to severe skin infections.
Patients must meet certain criteria, which can entail living within 30 minutes of the hospital, in case of emergencies; having running water, heat, AC, and electricity; and often, not living alone, for help with basics like opening the door for care team members or making pharmacy runs. Importantly, hospital-at-home services are voluntary—never required.
“Patients absolutely love this program,” says Dr. Vivian Reyes, national physician lead for Kaiser Permanente’s Care at Home initiative, available in four states, including Oregon, where Watzig, a Kaiser Permanente member, encountered it.
They can sit in their favorite chair. Sleep in their own bed. Be with beloved pets and family—Watzig gets choked up describing what it meant having his three young sons by his side. They can enjoy their garden between treatments, as one of Reyes’ patients did. Eat home-cooked meals. Watzig’s wife, a trained chef, made him cod with chard after they submitted a shopping list packed with liver-friendly ingredients; a few hours later, groceries arrived at their doorstep, a free perk of Kaiser Permanente’s program.
Once recovered, patients are typically “discharged,” as with any hospitalization.

Home is where the … hospital is?
The concept isn’t exactly new. It was happening overseas and was pioneered in the U.S. by Dr. Bruce Leff, a geriatrician and researcher at the Johns Hopkins University School of Medicine. Back in the late ’80s, when he was a resident making house calls to elderly adults, he noticed that many of his patients—even those who’d just had heart attacks—were refusing to go to the hospital.
Leff still carries around a slide of one of them, Walter, a retired steelworker who lived with his cat in Baltimore. During a home visit, Leff discovered that Walter had clearly developed pneumonia, on top of his existing heart failure and COPD. “I said, ‘Walter, you need to go to the hospital because you’re really sick.’ And he looked at us and said—and I’ll never forget this—‘I’m so sick and tired of you geniuses from Hopkins. You’re great doctors, but you run a really shitty hotel.’” So Leff and his colleagues brought care to Walter.
Hospitals can be risky places, particularly for elderly adults, Leff explains. Falls happen more often in unfamiliar quarters. Superbugs break out. Sleep can suffer from constant interruptions and alarm bells. Delirium can set in, raising the risk for long-term cognitive issues, he says. “It’s very common for older adults to decline in their ability to function strictly because of the hospital environment,” Leff says. “That motivated us to think about developing a true hospital-at-home model.”
Leff made it his mission to do just that, piloting the concept in a small group of patients at Hopkins and then expanding it to patients within the Department of Veterans Affairs, among other avenues, as part of a national demonstration study. His research consistently showed positive outcomes, even without the high-tech telemedicine capabilities of today. Patients opted in at high rates. They had fewer complications like delirium, and a better experience compared to traditional inpatient stays. Cost of care was lower.
Leff got to work trying to spread the model nationwide by sharing tools and best practices with other hospitals. “You don’t want to do this with Scotch Tape and Post-it Notes. It really has to be built out” to be done well and safely, he says. New Mexico’s Presbyterian Healthcare Services eventually rolled out an initiative with his help, as did Mount Sinai in New York. The movement was full of potential, and stood to benefit patients well beyond the elderly, he says.
There was just one big problem: Hospitals had very few ways to get reimbursed for providing hospital-at-home care, since commercial insurers and traditional government payers largely hadn’t stepped up to the plate. “Uptake was very slow,” Leff says. Until “COVID hits, and the world goes nuts.”
Read More: Long Waits, Short Appointments, Huge Bills: U.S. Health Care Is Causing Patient Burnout
A home run?
All of a sudden, in March 2020, “hospitals were trying to figure out what are we going to do with all these very sick patients? We don’t have room,” Hole says. Contagion was a grave concern. Field hospitals were being set up in convention centers and on ships. Solutions were urgently needed.
In response to the pandemic, the Centers for Medicare & Medicaid Services (CMS)—the nation’s largest payer for health care services—provided regulatory flexibility allowing hospitals to offer inpatient-level care outside of the traditional hospital setting, including within people’s homes—and be reimbursed for doing so. The initiative was expanded into the Acute Hospital Care at Home waiver program, to which hospitals must apply, and that Congress extended through Dec. 31, 2024.
What happens next is also up to Congress.
As of late August 2023, CMS had authorized 296 hospitals and 125 health systems in 37 states to offer acute hospital care at home. Although many hospitals haven’t gone beyond the application stage—“it’s a pretty heavy lift to stand up a program,” Hole says, compounded by reluctance tied to the waiver’s uncertain future—interest is proliferating.
“There’s always going to be reasons you have to go to the hospital, right? We’re not going to mail you an open heart surgery kit,” says Mark Howell, director of policy for the American Hospital Association, which is ultimately advocating for a permanent program regulated by CMS and operated by hospitals. “My biggest fear, though, is that if the waiver is not extended, you lose a lot of momentum,” at a time when “there’s a chance to really change the way we deliver health care in a very innovative way.”
The vast majority of programs would have to shut down, he says, unless they’re run by payer-providers, like Kaiser Permanente, or have other arrangements. But if the federal government were to give it a seal of permanency, the hope is that more state regulatory authorities and commercial insurers would get on board, Howell says.
In addition to a growing pile of evidence suggests that hospital at home can produce similar, if not better, outcomes than traditional inpatient hospitalization in many domains, proponents say the model has potential to expand health care access to underserved communities (think: rural America) while addressing some of the social factors that can hinder patients’ well-being. “You get a glimpse into their lives that you can’t possibly get when they’re in a brick-and-mortar hospital,” Reyes says.
Is there food in the refrigerator or could hunger be an issue? Mold that’s making asthma worse? Is transportation available? “We can identify those barriers and address them,” says Dr. Cheng-Kai Kao, physician leader of the University of Chicago Medicine Hospital at Home program, which recently launched after more than a year of preparation.

A different view
While some experts describe this as the future of health care, others reject that notion. “We are really disturbed by this trend,” says Michelle Mahon, a registered nurse and the assistant director of nursing practice for National Nurses United, the country’s largest union of registered nurses. NNU calls these programs “home all alone” and has published a report condemning the CMS waiver initiative.
She says the idea that acute care patients—who could experience an urgent decline at any moment—can be cared for at home versus the hospital, where highly trained registered nurses vigilant for subtle signs of trouble are at the bedside 24/7, “is absolutely preposterous, and more importantly, dangerous.” The union views the movement as an effort by the health care industry to maximize profits at the expense of patients, replacing skilled labor with technology, she says.
Susan Reinhard, senior vice president and director of AARP’s Public Policy Institute, has a different concern: the impact on family caregivers. A nurse and “proponent of care at home,” Reinhard’s previous research has shown that family caregivers often feel overwhelmed and unprepared to help loved ones—who’ve chosen to age in place, say, versus move into a nursing home—manage even basic health conditions.
That’s why AARP helped push through legislation in 45 states requiring hospitals to educate caregivers on the medical tasks they may need to handle once a loved one is discharged from a usual hospital stay, she explains. (Those requirements aren’t yet baked into hospital-at-home programs, she says.)
While advocates say these programs are set up to minimize family involvement, leaving most tasks to the professionals, Reinhard wonders to what degree caregivers are involved in the decision to elect hospital at home when the option is presented to patients. Do they have a say, she asks? Do they know what they’re signing up for? Who’s helping patients get to the bathroom? Bathe? Change the sheets? Do laundry—all of the services hospitals provide, she asks?
Reinhard is currently surveying hospital-at-home caregivers to better understand their views and needs. “This is a changing model of care,” she says. “When you have something new, you have to keep asking questions.”
Now six months out from a liver transplant, Watzig is thriving. He says his health is restored and he’s grateful to be alive. Two month-apart hospital-at-home stints helped him hang on during a dark time, until it became evident that a new organ was the only path forward. A time when he couldn’t tolerate the idea of being traditionally hospitalized. Says Watzig: “I am telling you—and this is not hyperbole—it literally saved my life.”